70
60
70
NORMAL VALUES
LA area – 2 chamber
MALE: MEAN±SD: 21±5cm2, Lower limit – Upper limit: 12-30
FEMALE: MEAN±SD: 19±5cm2, Lower limit – Upper limit: 10-28
LA area – 4 chamber
MALE: MEAN±SD: 23±5cm2, Lower limit – Upper limit: 13-32
FEMALE: MEAN±SD: 21±4cm2, Lower limit – Upper limit: 13-29
LA volume
MALE: MEAN±SD: 72±20ml, Lower limit – Upper limit: 31-112
FEMALE: MEAN±SD: 64±18ml, Lower limit – Upper limit: 28-100
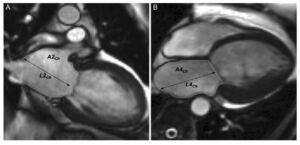
The Biplane Area-Length method, also known as the B-Planer method, is a technique used to measure left atrial volume using cardiovascular magnetic resonance (CMR) imaging. This method involves acquiring images in the horizontal and vertical long-axis cines to measure left atrial end-systolic areas and longitudinal dimensions.[1]
- The above areas are segmented at the end of ventricular systole – when the left atrium is the biggest and just before the opening of the mitral valve.
- The atrial endocardial border should be traced to determine LA area with the exclusion of the pulmonary veins and mitral valve recess. The normal values can vary depending on the inclusion or exclusion of atrial appendage.
- The normal values mentioned exclude LA appendage in segmentation.
The Biplane Area-Length method is based on the assumption that the left atrium is shaped like an ellipsoid. The left atrial volume is then calculated using the formula: 8/3π * (Area1 * Area2 / Length), where Area1 and Area2 are the maximum areas of the left atrium in the four-chamber and two-chamber views, respectively, and Length is the shortest left atrial dimension measured in either view.[1]
This method has been shown to be effective for evaluating left atrial volumes and ejection fraction in both normal subjects and patients with atrial fibrillation.[1] It has also been found to be highly reproducible and accurate, with good interobserver agreement.[1]
References
- SCMR Position Paper (2020) on Clinical Indications for Cardiovascular Magnetic Resonance. Leiner T, Bogaert J, Friedrich MG, et al. Journal of Cardiovascular Magnetic Resonance : Official Journal of the Society for Cardiovascular Magnetic Resonance. 2020;22(1):76. doi:10.1186/s12968-020-00682-4.
45%
20
Male Female
Cardiac Magnetic Resonance (CMR) derived Left Ventricular Filling Pressure (LVFP) is a significant tool in the assessment and prognosis of heart failure (HF). Studies have shown that elevated CMR-derived LVFP is strongly associated with symptoms and signs of HF, such as pleural effusions, orthopnoea, lower limb oedema, and breathlessness.(1) Furthermore, raised CMR-derived LVFP is independently associated with subsequent HF hospitalization and major adverse cardiovascular events (MACE).[1]
CMR can estimate LVFP in patients with suspected HF, and this CMR-modelled LVFP has been shown to have prognostic power(2). It was found to be superior to transthoracic echocardiography in classifying patients as having normal or raised filling pressures and was associated with an increased risk of death.
In addition to its role in HF, CMR-derived LVFP can also be used to measure acute and dynamic changes in preloading conditions on the left ventricle during adenosine-administered first-pass perfusion CMR, which has been observed to rise significantly (3). In conclusion, CMR-derived LVFP is a valuable tool in the diagnosis, management, and prognosis of HF and other cardiovascular conditions. It provides critical insights into the patient’s condition and can guide therapeutic decisions.
There was a bias issue with the previously published equation to estimate PCWP by CMR which impacted its accuracy especially in females due to lower left ventricular mass than males. This has been addressed in a follow-up paper (4). The new equation which factors in the sex of the patient has been tested in the UK Biobank where raised CMR-modelled PCWP was an independent risk factor for incident heart failure and MACE in the general population (5).
References
- Grafton-Clarke C, Garg P, Swift AJ, Alabed S, Thomson R, Aung N, et al. Cardiac magnetic resonance left ventricular filling pressure is linked to symptoms, signs and prognosis in heart failure. ESC Heart Fail. 2023 Oct;10(5):3067–76.
- Garg P, Gosling R, Swoboda P, Jones R, Rothman A, Wild JM, et al. Cardiac magnetic resonance identifies raised left ventricular filling pressure: prognostic implications. Eur Heart J. 2022 May 4;ehac207.
- Garg P, Javed W, Assadi H, Alabed S, Grafton-Clarke C, Swift AJ, et al. An acute increase in Left Atrial volume and left ventricular filling pressure during Adenosine administered myocardial hyperaemia: CMR First-Pass Perfusion Study. BMC Cardiovasc Disord. 2023 May 11;23(1):246.
- Garg P, Grafton-Clarke C, Matthews G, Swoboda P, Zhong L, Aung N, et al. Sex-specific cardiac magnetic resonance pulmonary capillary wedge pressure. Eur Heart J Open. 2024 May;4(3):oeae038.
- Thomson RJ, Grafton-Clarke C, Matthews G, Swoboda PP, Swift AJ, Frangi A, et al. Risk factors for raised left ventricular filling pressure by cardiovascular magnetic resonance: Prognostic insights. ESC Heart Fail. 2024 Aug 12;
70
Mitral Regurgitation Fraction (%): 0%
- Use of Cardiac Magnetic Resonance Imaging in Assessing Mitral Regurgitation: Current Evidence. Uretsky S, Argulian E, Narula J, Wolff SD. Journal of the American College of Cardiology. 2018;71(5):547-563. doi:10.1016/j.jacc.2017.12.009.
- Assessment of Mitral Valve Regurgitation by Cardiovascular Magnetic Resonance Imaging. Garg P, Swift AJ, Zhong L, et al. Nature Reviews. Cardiology. 2020;17(5):298-312. doi:10.1038/s41569-019-0305-z.
- 2020 ACC/AHA Guideline for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Otto CM, Nishimura RA, Bonow RO, et al. Journal of the American College of Cardiology. 2021;77(4):e25-e197. doi:10.1016/j.jacc.2020.11.018.
- Usefulness of Mitral Regurgitant Volume Quantified Using Magnetic Resonance Imaging to Predict Left Ventricular Remodeling After Mitral Valve “Correction”. Uretsky S, Shah DJ, Lasam G, et al. The American Journal of Cardiology. 2020;125(11):1666-1672. doi:10.1016/j.amjcard.2020.02.045.
- Discordance Between Echocardiography and MRI in the Assessment of Mitral Regurgitation Severity: A Prospective Multicenter Trial. Uretsky S, Gillam L, Lang R, et al. Journal of the American College of Cardiology. 2015;65(11):1078-88. doi:10.1016/j.jacc.2014.12.047.
- Mitral Annular Disease at Cardiac MRI: What to Know and Look For. Silva Ferreira MV, Soares CSP, Araujo-Filho JAB, et al. Radiographics : A Review Publication of the Radiological Society of North America, Inc. 2024;44(7):e230156. doi:10.1148/rg.230156.
20 ml
Aortic Regurgitation Fraction (ARF) (%): 0%
Cardiac magnetic resonance imaging (CMR) offers several benefits over echocardiography in the assessment of aortic regurgitation (AR), particularly in its ability to provide accurate and reproducible quantification of regurgitant volume and regurgitant fraction.
Firstly, CMR provides absolute regurgitant volumes and fractions irrespective of the number, eccentricity, or type of regurgitant jets, which can be challenging to assess accurately with echocardiography. This is particularly advantageous in cases of prosthetic valve regurgitation, where echocardiography may underestimate the severity of regurgitation due to technical limitations.[1]
Secondly, CMR allows for direct measurement of both antegrade and retrograde flow using phase-contrast imaging, which is not affected by the variability in the shape of the regurgitant orifice during the cardiac cycle, a common limitation in echocardiography. This results in more consistent and reproducible measurements.[2]
Additionally, CMR provides comprehensive assessment of left ventricular (LV) volume, LV systolic function, and aortic morphology, which are crucial for determining the timing of surgical intervention in AR patients.
Studies have demonstrated that CMR-derived parameters, such as regurgitant fraction and LV end-diastolic volume, are strong predictors of clinical outcomes, including the need for surgery and the development of heart failure symptoms.[3] This predictive capability underscores the clinical utility of CMR in managing AR.
Recent studies have shown that CMR-derived LV end-systolic volume index (LVESVi) and indexed LV end-diastolic volume (LVEDVi) are strong predictors of clinical outcomes in AR patients. Specifically, an LVESVi ≥ 43 mL/m² and an LVEDVi ≥ 109 mL/m² are associated with worse outcomes, providing additional discrimination over traditional diameter measurements.[4]
References
- Guidelines for the Evaluation of Prosthetic Valve Function With Cardiovascular Imaging: A Report From the American Society of Echocardiography Developed in Collaboration With the Society for Cardiovascular Magnetic Resonance and the Society of Cardiovascular Computed Tomography. Zoghbi WA, Jone PN, Chamsi-Pasha MA, et al. Journal of the American Society of Echocardiography : Official Publication of the American Society of Echocardiography. 2024;37(1):2-63. doi:10.1016/j.echo.2023.10.004.
- Guidelines for the Evaluation of Valvular Regurgitation After Percutaneous Valve Repair or Replacement: A Report From the American Society of Echocardiography Developed in Collaboration With the Society for Cardiovascular Angiography and Interventions, Japanese Society of Echocardiography, and Society for Cardiovascular Magnetic Resonance. Zoghbi WA, Asch FM, Bruce C, et al. Journal of the American Society of Echocardiography : Official Publication of the American Society of Echocardiography. 2019;32(4):431-475. doi:10.1016/j.echo.2019.01.003.
- A Comparison of the Clinical Efficacy of Echocardiography and Magnetic Resonance for Chronic Aortic Regurgitation. Postigo A, Pérez-David E, Revilla A, et al. European Heart Journal. Cardiovascular Imaging. 2022;23(3):392-401. doi:10.1093/ehjci/jeaa338.
- Influence of Cardiac Remodeling on Clinical Outcomes in Patients With Aortic Regurgitation. Malahfji M, Crudo V, Kaolawanich Y, et al. Journal of the American College of Cardiology. 2023;81(19):1885-1898. doi:10.1016/j.jacc.2023.03.001.
Author
Dr Pankaj Garg MD MRCP FRCP FESC
Disclaimer:
- These calculators are for educational and informative purposes ONLY.
- The calculators provided are not meant to be a substitute for professional advice.
- The information provided is not to be used for medical diagnosis.
- The authors make no claims of the accuracy of the information contained herein.
- The authors make no claims whatsoever, expressed or implied, about the authenticity, accuracy, reliability, completeness, or timeliness of the material, software, text, graphics, and links given.
- In no event shall the authors, its suppliers, affiliates, or any third parties be liable in any manner whatsoever for any damage arising upon use of any information provided.
Link to Android version: Download Here.

